This section discusses the basics of burn protection and Legionella control. Later sections describe specific hardware that can be used to achieve the water temperatures necessary for safe and sanitary delivery of domestic hot water.
INTRODUCTION
The temperature at which domestic hot water is distributed through building plumbing systems can have profound implications on human health and safety. The DHW must be at a temperature that is appropriate for the intended use. For example, when hot water is used for washing and sanitizing food processing equipment, its minimum temperature is often mandated by law.
In the U.S., the Food and Drug Administration typically requires a minimum water temperature of 180ºF for such purposes. Commercial or institutional laundry facilities typically require domestic hot water at temperatures ranging from 140 to 160ºF. The water supplied to patient rooms in hospitals or long-term health care facilities is also governed by law, and typically limited to 110ºF.
The temperature of domestic water also impacts the ability of undesirable and potentially dangerous microorganisms to survive and multiply. Water delivery temperatures that are typically acceptable and comfortable for skin contact range from 100 to 120ºF. However, this temperature range is also conducive to growth of certain microbes, most notably Legionella bacteria.
This section discusses the basics of burn protection and Legionella control. Later sections describe specific hardware that can be used to achieve the water temperatures necessary for safe and sanitary delivery of domestic hot water.
BURN PROTECTION
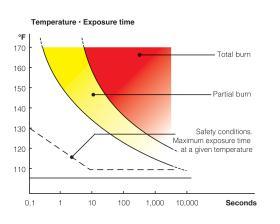
One of the greatest potential hazards associated with domestic hot water systems is the risk of moderate to severe burns when skin is exposed to water at high temperatures in sinks, showers, bathtubs or other fixtures. The ability of hot water to burn human skin depends on its temperature and exposure time. It also depends on age. Children’s skin is more vulnerable to rapid burns from overly heated water. The higher the water temperature, the shorter the time required to produce a burn of a given severity. Figure 2-2 shows how burn severity of adult skin is affected by water temperature and exposure time.
While it may seem intuitive to never set the temperature controls that regulate domestic water heating above a maximum safe temperature, such as 110ºF, there are circumstances where this is not possible.
For example, the DHW systems in restaurants or other facilities involved in food handling or preparation may require water temperatures of 180ºF to ensure disinfection occurs in dishwashing or cleaning of other food-processing equipment. However, if domestic hot water is supplied to a washroom lavatory in that same building, and the hot water supply piping to that lavatory is simply teed into the higher-temperature hot water supply piping, scalding hot water will be delivered to the lavatory faucet.
The potential for serious burns, as well as subsequent legal action by those affected, represents a major liability to the building owner. Prudence requires that such situations are not inadvertently created, and that existing situations with such piping be corrected as soon as possible.
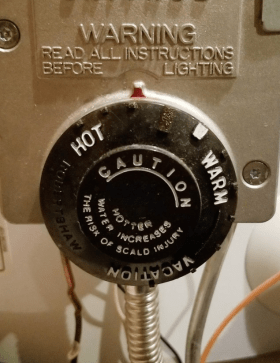
The low-cost, mass-produced mechanical thermostatic devices that control energy input to most tank-type water heaters do not provide precise adjustment of the water temperature leaving that device. Some do not have specific temperature settings printed on their adjustment dials. Subjective labels such as “hot,” “warm,” or “vacation,” do not allow those adjusting the water heater to make accurate settings to predetermined temperatures.
Tank thermostats that do have temperatures printed on their thermostat dials often produce leaving water temperatures that are significantly different from the dial setting. A 10ºF difference in outlet water temperature could make the difference between safe delivery of domestic hot water and the potential for a serious burn.
Most water heaters also provide easy access to temperature regulating controls. These controls are readily accessible on most gas-fired water heaters, as seen in Figure 2-4. A screwdriver is usually the only tool required for making thermostat adjustments on electric water heaters. This creates the potential for “unauthorized” tampering, and a subsequent major change in delivered water temperature to other occupants of the building, especially if multiple dwelling units are served from a common water heater.
Adjusting the water heater thermostat to a higher-temperature setting is often the perceived solution for inadequate DHW delivery, especially when occupants are unsatisfied with the water heater’s performance following a period of high demand. While increasing the temperature setting of the water heater does store more heat in the tank, and thus, makes longer DHW draws possible, it is often done without installation of suitable temperature-limiting devices between the water heater and fixtures.
It may also seem intuitive that those using a fixture receiving overly heated water would quickly adjust the flow of hot versus cold water to achieve a safe mixed temperature. This approach was used for decades in thousands of buildings, and is still the only method of water-temperature control at many fixtures. However, the reaction time and lack of caution of young children and elderly adults may not be adequate to prevent scalding hot water from causing burns, especially when that water is drawn from unfamiliar fixtures at hotels, restaurants or other commercial/recreational facilities.
Another possibility is hot water provided from heat sources such as solar thermal collectors or biomass boiler systems that can operate over a wide range of temperatures. Domestic hot water supplied directly from a solar thermal system could be at 110ºF one day, and perhaps 170ºF by the end of the following sunny day. Similarly, the water temperature supplied by a heat exchanger in a thermal storage tank connected to a wood-fired boiler could vary considerably depending on how that boiler is operated.
For these reasons it is essential to provide accurate and reliable temperature protection between any source of domestic hot water and fixtures where that water will come in contact with skin. The consequences of serious and possibly irreversible burns caused by overheated domestic water should never be taken lightly.
In addition to the potentially life-changing medical issues faced by the victim, there is the legal liability associated with designing, installing or adjusting the domestic water-heating system that caused the burn. It is therefore a highly recommended and often mandated practice to equip all domestic hot water systems with devices that can reliably protect against such conditions.
BIOLOGICAL CONTAMINANTS
There are several types of microorganisms that can be present in domestic plumbing systems. Examples are biological or microbial contaminants such as bacteria, viruses, protozoa and parasites. The source of the water often determines the probability and concentration of such contaminants.
Private wells that are dug or driven (versus drilled) can be relatively shallow, and as such more subject to biological (and chemical) contaminants present on ground surfaces or just beneath the surface. Possible sources for biological contaminants include animal feces, microbes associated with decaying plant matter, decaying remains of small vermin, and seepage from septic systems.
Equipment is available to reduce biological contamination in private water systems. This includes chemical injection devices as well as carbon filters and devices that expose water to ultraviolet light. The extent to which these devices are used often depends on building owner attitudes, budgets and tested levels of contaminants. Such devices and treatment processes are not mandated by code or regulation in many regions of North America.
Water supplied from public water systems undergoes continuous monitoring for both biological and chemical contaminants, and is subsequently treated to reduce the level of such contaminants to legally required standards. This monitoring and treatment is essential, especially considering that such systems directly impact the health of thousands of people.
LEGIONELLA BACTERIA
Still, even when private or public water treatment systems are used, some microbes can survive and subsequently multiply in domestic hot water systems. One such microbe is Legionella bacteria. These bacteria are naturally present in rivers, lakes, wells or stagnant pools of water, and as such, are inevitably present to some degree in many private water supply systems. Legionella bacterial is also found in municipal water mains and can, to some extent, survive municipal water treatment processes.
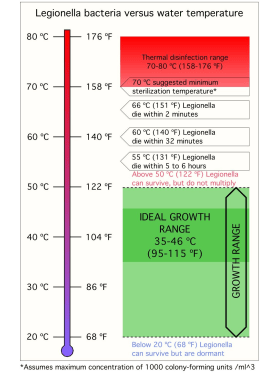
Legionella bacteria can multiply in water at temperatures between 68 and 122ºF. Below 68ºF, the bacteria are present, but remain dormant. Warm water between 95 and 115ºF provides an optimum growth environment for Legionella bacteria. Growth is aided by the presence of biofilms in pipes or tanks, mineral scale, sediment or other microorganisms within plumbing systems. Dead-leg plumbing systems that harbor stagnant water also provide an enhanced growth environment and should be avoided.
Figure 2-7 shows the temperatures under which Legionella bacteria can survive, or be killed. Given the right conditions, Legionella bacteria can cause two diseases in humans:
• Pontiac fever, which develops after an incubation period of 1 to 2 days. Its symptoms include fever, muscle aches, headache and, in some cases, intestinal complaints. This form of Legionella infection is often mistaken as the common flu and usually runs its course in 2 to 5 days without need of antibiotic treatment.
• Legionnaires’ disease, which was first identified after a 1976 outbreak of pneumonia at a Philadelphia hotel where an American Legion convention was being held. The outbreak affected 221 people and led to 34 deaths.
Legionnaires’ disease develops after an incubation period of 2 to 10 days (5 or 6 days on average). Symptoms may include high fever, muscle aches, diarrhea, headache, chest pain, cough, impaired kidney function, mental confusion, disorientation and lethargy. Legionnaires’ disease is difficult to distinguish from pneumonia. Treatment involves a course of antibiotics. Legionnaires’ disease can be fatal, especially if diagnosed late or involving patients that are older, weak or have depressed immune systems.
Legionnaires’ disease is contracted by inhaling a sufficient amount of ultra-fine water droplets (1 to 5 microns in diameter) that contain Legionella bacteria. Such droplets can be produced by shower heads, faucets, spas, humidifiers, decorative fountains and cooling towers. Legionnaires’ disease is not passed from person to person, nor acquired by drinking water containing Legionella bacteria.
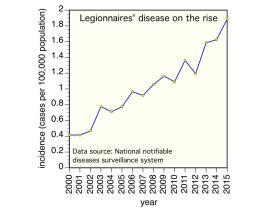
The rate of reported cases of legionellosis, which comprises both Legionnaires’ disease and Pontiac fever, has increased 286% in the United States during 2000–2014. Approximately 5,000 cases were reported to the Centers for Disease Control and Prevention (CDC) in 2014. Approximately 9% of reported legionellosis cases are fatal.1
LEGIONELLA CONTROL
Since Legionella was first identified as a serious health hazard following an outbreak at the 1976 American Legion convention in Philadelphia, various means of minimizing the health risks associated with Legionella bacteria have been developed.
Current Legionella mitigation requirements in the United States include a mandate issued in June 2017 from the Centers for Medicare and Medicaid Services (CMS).2
This mandate requires Medicare and Medicaid facilities to implement water testing and management plans that conform to ASHRAE Standard 188 Legionellosis: Risk Management for Building Water Systems, June 26, 2015.
Recent studies by the Center for Disease Control have determined that 19 percent of Legionnaires’ disease outbreaks were associated with long-term care facilities and 15 percent with hospitals.
Legionella bacteria can be maintained at acceptable levels using several techniques, including:
• Injection of chemical biocides (chlorine and chlorine dioxide)
• Periodic flushing of all plumbing systems
• Exposure to intense ultraviolet light
• Exposure to ozone
• Thermal disinfection
The latter method is discussed in this issue of idronics.
THERMAL DISINFECTION
Although there are several methods for maintaining acceptably low levels of Legionella bacteria in domestic hot water systems, thermal disinfection is one of the simplest to execute. Thermal disinfection has been extensively used in European systems for over 15 years, and is currently the dominant method of Legionella control in Europe.
The basic concept of thermal disinfection is to periodically raise the hot water temperature throughout the hot distribution piping to a suitable level and maintain that temperature for a specified time, so that Legionella bacteria within the water, as well as within biofilms or scaling inside the piping system, will be killed.
Thermal disinfection provides the following advantages and benefits:
- There is no need to purchase, transport or store aggressive chemicals such as chlorine for on-site water treatment.
- There is no concern about over-dosing or under-dosing of disinfection chemicals.
- There is no need to flush plumbing after chemical dosing.
- There is no water wasted during thermal disinfection.
- There is no concern about human or animal sensitivity to disinfection chemicals.
- There is no need for cleaning the disinfection apparatus, as is required for UV light disinfection systems.
- There is no need to install or maintain “ultra-filtration” or membrane filtration equipment.
- There is no concern about the ability of ozone, which can be used as a disinfection chemical, to react with metals, polymers or elastomers in the system.
- In properly designed systems, there is no change in the water temperature or water chemistry at the fixtures during the disinfection process.
- There is no concern about potential corrosion of system components such as elastomers or metals due to exposure to higher levels of disinfection chemicals. Chlorine-based water-disinfection methods using chlorine, chloramine or chlorine dioxide have caused failure in plumbing systems using copper, polybutylene and PEX. Some of those failures have led to class action lawsuits.3
Figure 2-7 shows that maintaining water at a temperature of 140ºF kills Legionella bacteria in that water within 32 minutes. A water temperature of 151ºF reduces the kill time to 2 minutes. A water temperature of 158ºF or higher provides essentially immediate kill.
Although these temperatures can be attained by many domestic water-heating devices, they are all well above the temperatures that are considered safe for delivery of hot water at fixtures where contact with human skin is possible. Thus, the control of Legionella bacteria combined with the need to provide safe DHW delivery temperatures to fixtures requires multiple water temperatures at different locations and different times within the hot water system.
Legionella bacteria can live within tiny voids in biofilms or scale inside DHW distribution piping. These films and scale present thermal resistance to hot water passing through the system during a thermal disinfection cycle. It is therefore necessary to maintain the flow of elevated-temperature water for sufficient time to allow disinfection conditions to permeate through all films or scaling in the pipe.
It’s also important that the elevated water temperature required for thermal disinfection is distributed throughout the system.
Consider the situation where water is heated to a minimum thermal disinfection temperature, such as 140ºF, and circulated through the DHW system. Heat loss from piping causes the water temperature to drop, typically several degrees, as it passes through the recirculating system. Piping components near the end of the recirculation system may not achieve the necessary temperature/time conditions to ensure thorough disinfection. Thus, a constraining factor in achieving acceptable thermal disinfection is typically the temperature at the end of a DHW recirculation system.
The higher the temperature attained during a thermal disinfection cycle, the shorter its duration can be. In the absence of specific codes or standards that require otherwise, the following water temperatures and associated cycle durations have been commonly used for once-per-day disinfection of domestic hot water-delivery systems:
• At least 158ºF (70 ºC) maintained throughout the system for 10 minutes
• At least 149ºF (65 ºC) maintained throughout the system for 15 minutes
• At least 140ºF (60 ºC) maintained throughout the system for 30 minutes
All of these time and temperature criteria stipulate “throughout the system.” A thermal disinfection cycle would be considered incomplete if the water temperatures and cycle durations noted above were not achieved and maintained at the return of the recirculation loop, as well as elsewhere within the loop. The best designed systems take this into account by verifying that the thermal disinfection criteria have been maintained at the return end of the recirculation loop. Later sections describe specific hardware that facilitates this concept.
RECIRCULATING DHW SYSTEMS
Legionella bacteria are known to multiply at increasing rates in stagnant water. Ensuring movement of domestic hot water through the plumbing system minimizes the possibility of stagnant water. Although there is obviously movement when domestic hot water is drawn from a fixture, the total duration of these hot water draws is minimal relative to total elapsed time.
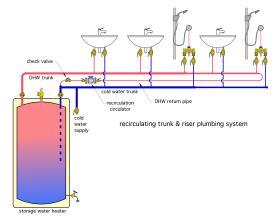
Adding a small stainless steel or bronze circulator and return piping to the system, as shown in Figure 2-9, creates consistent movement in the hot water recirculation portion of the system, which, depending on the operating times of the circulator, reduces the potential for stagnant water.
Recirculation also ensures that hot water is immediately available from fixtures served by the recirculating loop, and thus, improves owner satisfaction with the system. Use of a recirculating DHW delivery system is one of several “tactics” that can be used to limit potential growth of Legionella bacteria.
Recirculating hot water systems were covered in detail in idronics #21:
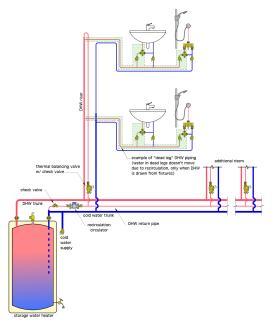
MINIMIZING "DEAD LEG" PLUMBING
Reducing stagnant water reduces potential growth environments for Legionella bacteria. Even in systems with recirculating loop piping, there is a potential for water to stagnate in pipes connected between that loop and the fixtures. These pipes are often referred to as “dead legs” in the system. Figure 2-10 shows the concept.
In larger buildings, domestic hot water-delivery systems may serve areas that have infrequent occupancy, or are used in ways that create long periods of no domestic hot water demand. These portions of plumbing systems are especially vulnerable to stagnant water, and thus, create potential breading areas for Legionella bacteria.
Plumbing system designers should make every effort to minimize the amount of piping in the system that could contain stagnant water.